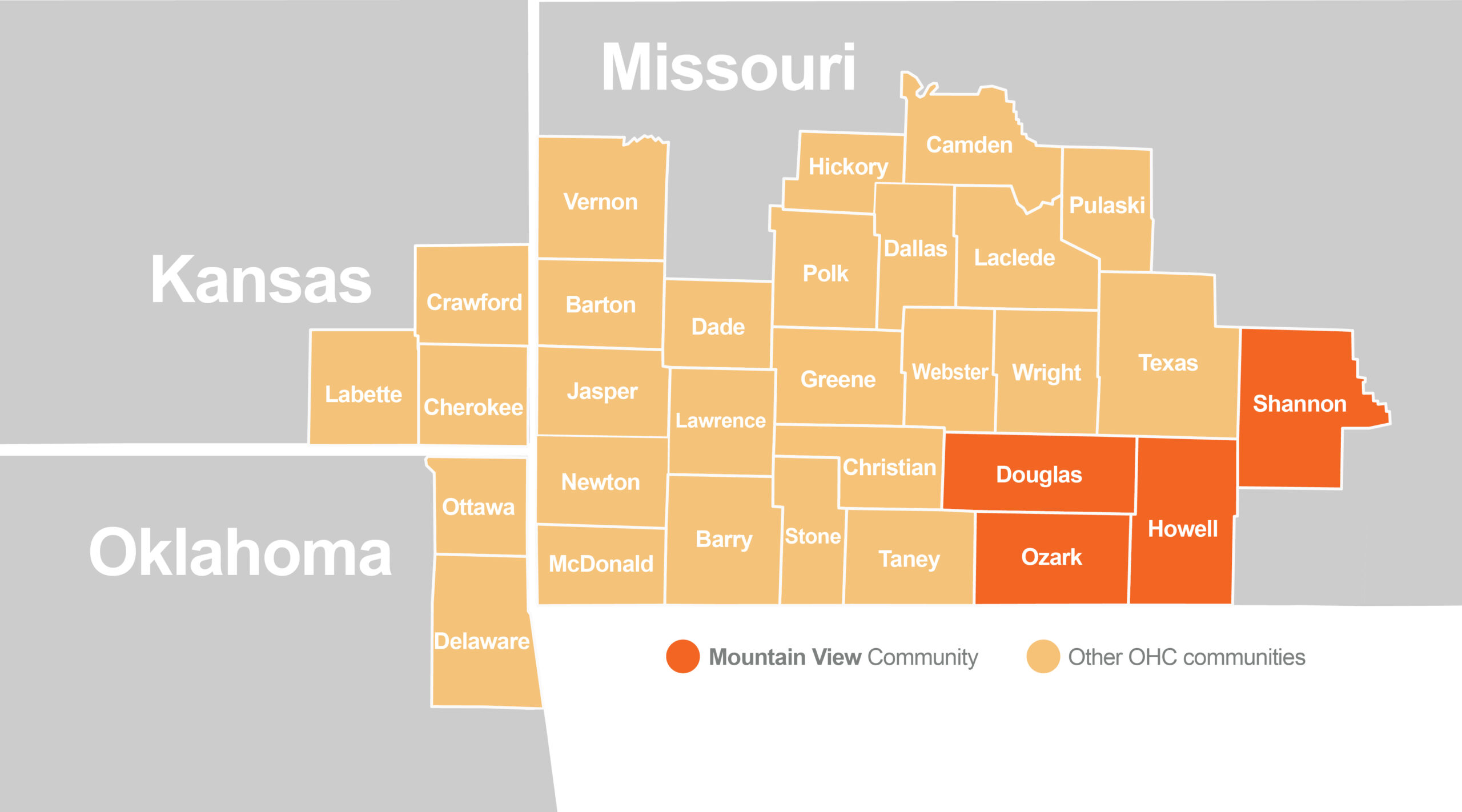
Service Area
The Mountain View Community is made up of 4 Missouri counties: Douglas, Ozark, Howell, and Shannon. The counties included in the Mountain View Community service area were based on the only participating hospital serving this area, Mercy Hospital St. Francis located in the City of Mountain View. Mercy Hospital system serves millions each year, Mercy is a cutting-edge healthcare provider that is charged with “providing the region with high-quality care and an experience that is easier and more personal.” Mercy Hospital Springfield houses 886 beds that serve people throughout Southwest Missouri and Northwest Arkansas.
West Plains, in Howell County, is the county seat. The population is over 12,000. As the largest city within 100 miles of south-central Missouri, it provides many conveniences and services to the area. Gainesville, with a population of less than 750 people, is the county seat of Ozark County. Ava is the county seat of Douglas County. Shannon County expands the distance of over 1000 square miles, making it the 2nd largest county in Missouri. The population is just over 8,000.
Population Overview
The Commission noted several important demographic and population trends within the 4-county Mountain View Community. This Community is home to 70,834 individuals, a decline of 7.4% between 2000 and 2010. A decline in population can cause concerns including aging populations, job losses, declining tax revenues and shrinking schools and neighborhoods. These effects can already be seen with nearly 23% of Community residents being minors under the age of 17, while approximately 36% are over the age of 55. Meaning, that the population is, on average, older than both the Region and nation. Older residents are more likely to be living with chronic illnesses and require access to more health services. Further, approximately 41% of the Community is within the age grouping of 18-64, which drives the workforce in the community.
Approximately 22% of the total population is living with a disability, which is higher than the regional rate at 17.3% and national rate of 12.62%. This may contribute to access to care and disparities amongst the disability community members. Factors that must be considered when planning for improvement in rural versus urban areas.
A few of these factors contribute to the overall vulnerability of the population of the Community. Vulnerable populations, such as people in poverty, minorities, and the elderly, often experience higher rates of chronic illness and worse health outcomes. To ensure vulnerable and at-risk populations were considered when identifying and addressing community health needs, the Commission identified them in each Community using the Center for Disease Control and Prevention (CDC) Social Vulnerability Index (SVI).
Using U.S. Census and American Community Survey data, the SVI identifies the most vulnerable groups across all comparative census tracts. Out of the highest vulnerability score of 1.0, the Mountain View Community has an overall SVI score of 0.6, meaning that it is more vulnerable than 60% of the rest of counties in the OHC Region. Scores for Socioeconomic Status (0.8), Household Composition and Disability (0.8), also demonstrate significant vulnerability of the local population. The Mountain View Community has higher rates of physical inactivity (29.2%), tobacco use (25.2%) and alcohol bingeing (17.5%) than the OHC Region, Missouri, and the U.S. These are all areas of concern which impact health outcomes.
What makes a population vulnerable?
| Douglas County | Howell County | Ozark County | Shannon County | Mountain View Community | ||
|---|---|---|---|---|---|---|
| Socio-Economic Status | Below Poverty | 0.82 | 0.85 | 0.96 | 1 | 0.91 |
| Unemployed | 0.71 | 0.41 | 0.83 | 0.73 | 0.67 | |
| Income | 0.94 | 0.83 | 0.96 | 0.99 | 0.93 | |
| No High School Diploma | 0.84 | 0.43 | 0.79 | 0.86 | 0.73 | |
| Household Composition & Disability | Aged 65+ | 0.89 | 0.55 | 0.96 | 0.73 | 0.78 |
| Under Age 18 | 0.23 | 0.64 | 0.08 | 0.28 | 0.31 | |
| Disability Status | 0.77 | 0.81 | 0.77 | 0.95 | 0.82 | |
| Single-Parent Households | 0.05 | 0.43 | 0.1 | 0.47 | 0.26 | |
| Minority Status & Language | Minority | 0 | 0.38 | 0.15 | 0.47 | 0.25 |
| Speaks English “Less than Well” | 0.68 | 0.32 | 0 | 0 | 0.25 | |
| Housing Type & Transportation | Multi-Unit Structures | 0.25 | 0.79 | 0.2 | 0 | 0.31 |
| Mobile Homes | 0.62 | 0.82 | 0.89 | 0.95 | 0.82 | |
| Crowding | 0.89 | 0.56 | 0.69 | 0.83 | 0.75 | |
| No Vehicle | 0.04 | 0.77 | 0.46 | 0.11 | 0.35 | |
| Group Quarters | 0.09 | 0.26 | 0.22 | 0.26 | 0.21 | |
| Orange highlight: The population in this county is more vulnerable than 90% of all other counties in its respective state. | ||||||
| Blue highlight: The population in this county is more vulnerable than 85% of all other counties in its respective state. | ||||||
| Beige highlight: The population in this county is more vulnerable than 80% of all other counties in its respective state. | ||||||
indicative of greater vulnerability. Percentiles are from the CDC’s SVI data.
Assessed Health Issues
Commission stakeholders began the RHA process with analysis of publicly available health data (secondary data) and participating health systems’ emergency room utilization data (primary data) to identify health issues of greatest concern across the region. The result was a ranked list of eight Ozarks Health Commission Region health issues. A full description of the health issues and indicators used can be found in the OHC Regional Health Assessment.
To represent diverse views from across the region and population, qualitative data was garnered. Across the OHC Region, these viewpoints were solicited via 75 individual interviews, 10 focus groups and 2,638 surveys. Methodologies used for the initial scoring/ranking of the health issues and the full report of the qualitative work can be found in the OHC Regional Report. This prioritization information can be used by organizations to develop community health improvement plans, guide decision making, and foster collaboration across initiatives for collective community impact.
During September and October 2021, twelve individual interviews, in addition to two virtual focus group discussions in the 4-county Community were completed. Those interviewed represented health and social service organizations, education and community collaboratives.
Of the 2,628 survey respondents from the Region, 8.65% indicated they lived in the Mountain View Community. Respondents were asked to rank perceived community needs, and the top 10 that emerged were:
- Drug and other substance abuse treatment and rehabilitation services, including detox
- Emergency mental health services for issues such as suicidal thinking or actions, homicidal thinking or actions, self-harm, or harm to others
- Integrated care, or where people can get medical care and counseling at the same time
- Affordable, quality childcare
- Drug and other substance abuse, education, prevention, and early intervention services
- Coordination of patient care between the hospital and other clinics, private doctors, or others
- Counseling services for mental health issues such as depression, anxiety, trauma, or others for adults
- Counseling services for mental health issues such as depression, anxiety, trauma, or others for adolescents and children
- Affordable housing
- Social services (other than healthcare) for people experiencing homelessness
Those interviewed represented health and social service organizations, education and community collaboratives. Stakeholders, education and community individual interviews and focus groups agreed that a top challenge was access to mental health services and healthcare. This information was considered during the process of establishing health priorities for the Mountain View Community. Methodologies used for the initial scoring/ranking of the health issues and the full report of the qualitative work can be found in the OHC Regional Report. This prioritization information can be used by organizations to develop community health improvement plans, guide decision-making, and foster collaboration across initiatives.
Mountain View Community Health Priorities
(click a health priority below to learn more)
Each Commission Community convened stakeholders to assess the feasibility of addressing the health issues identified through primary and secondary data sources, and further illuminated the qualitative community feedback. In the Mountain View Community, this was organized by Molly Holtmann, Director of Community Health and Access for Mercy Hospital and was held virtually Thursday, January 13, with every effort made to invite all public health agencies, organizations engaged by Crescendo Consulting, CHC members and leaders of vulnerable and underrepresented communities.
Based on the eight health issues identified by the Commission using publicly available and participating health systems’ data, stakeholders from the Mountain View Community convened to further discuss top priorities for the community.
The feasibility of changing each issue and readiness to address each issue was assessed. Feasibility rankings were influenced by stakeholders’ perceptions of the readiness of the community to address an issue, existing initiatives or momentum, whether leadership was established around the condition, perceived feasibility to change, complexity of the issue and the time frame to improve the issue (within 2-3 years or more than 2-3 years). The higher the score, the more significant the impact of the condition on the community, and the more difficult the condition was to address.
Participants using a short survey, which was opened one week before the meeting, assessed feasibility. Survey responses equaled roughly 50% of the total weighted ranking for each health issue.
| Rank | Initial Ranking Emergency Department and Public Health Data | Final Ranking Emergency Department, Public and Feasibility Data | Rank Change | ||
|---|---|---|---|---|---|
| 1 | Oral Health | 3.78 | Oral Health | 3.10 | no change |
| 2 | Lung Disease | 3.30 | Heart Disease | 2.88 | +1 |
| 3 | Heart Disease | 3.17 | Lung Disease | 2.8 | -1 |
| 4 | COVID-19 | 2.83 | COVID-19 | 2.78 | no change |
| 5 | Diabetes | 2.67 | Diabetes | 2.55 | no change |
| 6 | Mental Health | 2.35 | Mental Health | 2.38 | no change |
| 7 | Cancer | 2.25 | Substance Use & Recovery | 2.27 | +1 |
| 8 | Substance Use & Recovery | 1.85 | Cancer | 2.26 | -1 |
Cancer
As the sixth leading cause of death worldwide, accounting for more than 10 million deaths in 2020, cancer is a significant health concern for many. This illness, which is the uncontrolled growth of abnormal or damaged cells, most commonly takes the form of breast, lung, colon and prostate cancers. Approximately one-third of cancer deaths result from health behaviors such as tobacco use, high body mass index, alcohol consumption, low fruit and vegetable intake, and a lack of physical activity. Cancer-causing infections, such as human papillomavirus (HPV) and hepatitis, are responsible for nearly three-in-ten cases of cancer in low- and lower-middle-income countries. This demonstrates that many social determinants of health found in the Mountain View Community contribute to this growing health issues. This also means that many causes of cancer could be prevented, and if found early and treated effectively, many cancers can be cured.
Early detection and treatment are an area for improvement in the Mountain View Community. The Community lags behind the OHC region, Missouri, and the U.S. in the number of pap smears, mammograms, and colorectal screenings conducted. The lower rate of screenings can be attributed, in part, to the high rate of uninsured adults. While the cancer incidence rate in the Mountain View Community is lower than the rates for the OHC Region, Missouri, and the U.S. at 368.9 cases per 100,000 residents, the cancer mortality rate is 8% higher than the state rate and 16% higher than the U.S. rate.
According to community focus groups, Cancer is gaining ground. Many participants cited cancer as a major and growing problem.
People think there’s something wrong with the water or other system in West Plains that makes them more susceptible to cancers.
mountain view Community Member
Over 40% of all cancer patients utilizing the hospitals are over the age of 65.
________
African Americans in the Mountain View community visit the emergency department with cancer diagnosis at double the rate of any other race group.
Substance Use & Recovery
When people got a lump sum of money, they could buy more drugs and they overdosed. Overdoses make up a small percent of transport volume, but they still saw a noticeable increase”
Mountain View Community member
Younger (under age 18) and older (over age 65) residents are less likely to be diagnosed with a substance abuse diagnosis in the Mountain View Community.
Substance use as a behavioral health disorder encompasses the use of intoxicating substances in a manner which negatively effects the persons global wellness. Recovery from substance use disorder is a process through which the individual improves that health and wellness, starts living a self-directed life and striving to reach a more fulfilling purpose. This comes in a variety of pathways, from public health and behavioral health providers, social supports, community resources and mutual aid. There are currently 22.75 million individuals openly in recovery in the US. Only 1 in 4 people needing substance use support and assistance will receive services.
When examining hospital utilization, public health and community input data, Substance use and recovery did not rise to top during the prioritization process. After considering that there are significant limitations in collecting and accessing secondary data for this analysis, community stakeholders determined that this assessed health issue was of great priority to the Mountain View Community. Qualitative information shared by both experts and members of the community helps illustrate that there is more of the story missing in the quantitative data. Even given these limitations, the prevalence of substance use is higher in the Mountain View Community than in the whole OHC Region, Missouri, and the U.S.
Through community input on substance use and recovery, education, prevention, access to treatment, detox and rehabilitation services were identified as top needs in the community. Community members stated that there is a stigma around seeking care for both mental health and substance use, and even when care is sought there are not enough inpatient beds. In hospital emergency departments, one in three patients paid through Medicaid, indicating a financial or lifestyle hardship for these patients. Concerningly, the second most comment method of payment for substance use related visits was self-pay. These issues were only exacerbated by the COVID-19 pandemic.
Diabetes
Diabetes is a chronic health condition that affects how your body turns food into energy. If you have diabetes, your body either doesn’t make enough insulin or is resistant to the effects of insulin, leading to high blood sugar levels in the bloodstream. Over time, this can cause damage to multiple organs in the body, including the eyes, nerves, blood vessels and kidneys. It can also increase the risk of cardiovascular disease, decrease the body’s immunity and lead to decreased life expectancy.
One in five adults in the U.S. have diabetes and do not know it. Diabetes was the seventh leading cause of death in the U.S. in 2019, accounting for 87,647 deaths annually. Direct medical costs and lost productivity attributed to diabetes was estimated to be $327 billion in 2017. The Mountain View Community has a higher rate of diabetes than the OHC Region, Missouri, and the U.S., and this issue continues to grow. Twenty-one percent more adults are diagnosed with diabetes in the Mountain View Community than the national average. Two of the four counties in the Mountain View Community, Douglas and Howell, continue to report increasing rates of adults with diabetes.
Some people can control their blood sugar levels with healthy eating and exercise. However, as diabetes progresses, people may need multiple medications to control their blood sugar levels.
Type 2 diabetes is the most common form of diabetes, accounting for 90-95% of diabetes cases. It develops over many years and is usually diagnosed in adults. More than one in three adults in the U.S. have prediabetes, but more than 80% are not aware they are prediabetic. In prediabetes, blood sugar levels are higher than normal, but not high enough to be diagnosed as type 2 diabetes.
The progression to diabetes can be prevented or delayed with dietary changes and an active lifestyle. However, all four counties in the Mountain View Community measure significantly worse in physical activity than the U.S. rate. Moreover, Douglas and Ozark counties have a higher rate of low food access at 37.6% and 36.9%, respectively, than the national rate of 22.2%. For those at-risk for, or living with, diabetes, the impact on blood sugar levels that an inadequate access to consistent and nutritious food can have increases the risk of complications. Once again, pointing to the significance that social determinants play in overall health status.
People don’t have primary care providers. This is a very rural area, and the cost of gas is high. People wait until the last minute to get care or end up in the emergency room and let problems go longer than they should.
Mountain view community member
Emergency room visit for diabetes or diabetes-related complications increased by 7.9% between 2018 and 2020.
________
Females are more likely to present in the emergency department with a diabetes-related diagnosis. It is the only assessed health issue, aside from lung disease, to skew female.
Special Health Issue: COVID-19
Coronavirus disease (COVID-19) is an infectious disease caused by the SARS-CoV-2 virus. Most people infected with the virus experience mild to moderate respiratory illness and recover without requiring special treatment. However, some become seriously ill and require more advanced medical care. People over the age of 64 and those with underlying medical conditions like cardiovascular disease, diabetes, chronic respiratory disease or cancer are more likely to develop serious illness. Even after recovery, some people may have post-COVID conditions. These conditions can present as different types and combinations of health problems for different lengths of time. Multiorgan effects can affect many body systems, including heart, lung, kidney, skin and neurologic functions.
We’ve been seeing residual effects of COVID – kidney disease, heart disease, PTSD. Nobody was prepared for that.
mountain view Community Member
Throughout the pandemic, the Mountain View Community saw a case rate 3% higher than the rest of Missouri. This was largely due to higher transmission in Howell County, resulting in a case rate 8% higher than the rest of the state and 4% worse than the U.S.
Moreover, deaths from COVID-19 were far more common in this Community, with a nearly 21% higher mortality rate compared to the state average and 11% higher than the national average. Douglas County accounts for much of this disparity, with a mortality rate 44% higher than the Missouri rate and nearly 37% higher than the national rate. While Shannon County saw around 17% fewer deaths than the state and 27% fewer than the nation.
COVID-19 was the reason for 3% of emergency department visits in the Monett Community, with 46% of patients paying for care through Medicare and 32% utilizing commercial insurance.
Comments from individual interviews and focus groups about the impact of COVID-19 for the Community showed concern that residents stopped visiting the ER, unless major emergency. Residents died from problems because they didn’t get the care they needed. It was also mentioned that “Covid hasn’t taken distrust away from providers – residents may not get the vaccine, but they’ll see their doctor for other reasons”.
A very high percentage (91.45%) of respondents have a family doctor, family dentist, family health center, or clinic for regular or annual medical or dental care. However, nearly one-third (30.61%) of people who needed care in the past year chose not to receive care. Respondents note that exercise and dietary habits have worsened during the pandemic. Two-thirds say that social isolation has worsened. Social isolation, as demonstrated in nationally reviewed research, leads to increased behavioral health issues, more acute chronic disease, and other factors. High priority communities (e.g., Hispanic communities, LGBTQ+, seniors, and others) are more widely impacted.
Though COVID-19 initially ranked fourth as an assessed health issue in the Community, when feasibility and readiness to change were factored in, it was determined by community stakeholders that there was already a strong system in place to continue to address screening, testing, contract tracing, vaccination and treatment. The ongoing efforts and the lack of confidence that the virus would continue to be a dominating issue over the next several years resulted in the determination that COVID-19 is not a priority health issue. However, the full impacts of the virus will be seen in the months and years to come, so it will be prudent to continue evaluation of its impact.
Social Determinants of Health
(click a social determinant of health below to learn more)
Additional data critical to understanding the health of the population and the vulnerability of the Community was discerned by examining six groupings classified as social determinants of health: Economic Stability, Education Access and Quality, Healthcare Access and Quality, Neighborhood and Built Environment, Social and Community Context and Health Behaviors. The social determinants of health have a major impact on people’s health, well-being, and quality of life while also contributing widely to health disparities and inequities. Twenty percent of a person’s health and well-being is related to access to care of quality of services provided. Rather, 80% is related to the physical environment (10%), social determinants of health (40%) and health behaviors (30%). Therefore, examination of these factors is important as they play a significant role in the impact the assessed health issues have on the Mountain View Community.
Economic Stability
In the United States, 3 in 10 people live in poverty, and many people can’t afford things like healthy foods, health care, and housing. People with steady employment are less likely to live in poverty and more likely to be healthy, but many people have trouble finding and keeping a job. People with disabilities, injuries, or conditions like arthritis may be especially limited in their ability to work. In addition, many people with steady work still don’t earn enough to afford the things they need to stay healthy.
In the Mountain View Community, close to half of residents (49.9%) live at or below 200% of the federal poverty level (FPL), meaning a family of four cannot earn more than $25,750 annually. The percentage of children living in poverty is much higher, at 62.2%.
In addition to living in poverty, many in the Mountain View Community struggle to find affordable housing. Twenty-six percent of those in the Community live in substandard housing according to the U.S. Census Bureau and 10.1% report a severe housing cost burden. Nearly 34% of citizens currently have affordable housing that is below 60% of the area median income (AMI). Community stakeholders note that housing costs in the Monett Community have outpaced salaries. There are long wait lists for lower cost rental housing, which is contributing to higher costs.
Education Access & Quality
Education can be an indicator of health, with persons with higher levels of education often living healthier and longer lives. More than 15% of adults over 25 years old in the Mountain View Community do not have a high school diploma. This is more than 5% worse than the state average and nearly 4% higher than the national rate. Moreover, the Mountain View Community struggles with community members achieving college degrees. Those receiving their associates degree or higher account for 22.7% of the population, which is nearly 40% below the state average and 45% below the national average.
Healthcare Access & Quality
Many people in the United States don’t get the health care services they need. About 1 in 10 people don’t have health insurance. In the Mountain View Community, the rate of uninsured is even higher, with more than 20% of adults and 8% of children not having health insurance. People without insurance are less likely to have a primary care provider, and they may not be able to afford the health care services and medications they need. In addition, people may not trust the healthcare system. Some reasons for this may include lack of cultural awareness by providers, feeling unwelcome or uncomfortable in traditional clinical settings, previous negative experiences with healthcare providers, insufficient accommodations for the disabled, language barriers or clinics not having convenient times or locations.
Those with the financial means to access healthcare in the Community have nearly 9% fewer primary care providers per 100,000 residents to seek services with than the rest of Missouri and more than 17% fewer the U.S. Moreover, the Community has nearly 38% fewer mental health care providers than the U.S. Overall, the Mountain View Community struggles with retaining and attracting healthcare providers, with 50% of residents living in Health Professional Shortage Areas. A rate that is nearly twice as high as the state and national rates.
Health Behaviors
Health behaviors include individual-level behaviors, often influenced by access or quality of services, that can impact the overall health of an individual or community. Measured health behaviors include physical activity, fruit and vegetable expenditures, smoking, alcohol binge drinking, sexually transmitted infection (STI) rates and the prevalence of HIV. These behaviors can affect a wide range of health, functioning, and quality-of-life outcomes and risks.
In the Mountain View Community, physical inactivity has increased slightly since the prior assessment in 2019. Nearly one in three (29.2%) residents report no leisure time physical activity, which is higher than below state and national averages.
Analysis of fruit and vegetable expenditures are a way of determining how many community members have the inclination and ability to enjoy healthy foods. In the Mountain View Community, a household spends just over $654 on fruits and vegetables (fresh, frozen, or canned), which is more than $90 less than the national average.
Additionally, the Mountain View Community has a smoking rate that is slightly higher than the state rate, and 8.2% higher than the national average.
Neighborhood & Built Environment
The neighborhoods people live in have a major impact on their health and well-being. Where we live affects the basics of our daily lives and health. When affordable housing is lacking it impacts families and where they can afford to live. In the Mountain View Community, nearly 26%% of community members live in substandard housing. The Community also reports nearly one in four of community members have limited/low access to food.
Moreover, 31 out of 100 households in the Mountain View Community have low or slow internet access, a rate higher than the OHC Region, Missouri, and the U.S. As evidenced by the Covid pandemic, this lack of connectivity can affect resident’s ability to learn, work, and play.
Social & Community Context
Health begins where we live, learn and play. Community connections and social relationships can have a major impact on their health and well-being. Many people face challenges and dangers they can’t control, like unsafe neighborhoods, discrimination or trouble affording the things they need. The Mountain View Community has total social vulnerability index (SVI) of 0.6, with 1.0 indicating the highest possible vulnerability. This is 45% higher than both state and national averages. SVI scores that are higher show areas that are more vulnerable to socio-economic factors that can influence their health choices and behaviors. A prime example of this is homelessness. In the Mountain View Community, 3.7% of elementary and secondary students have been identified as homeless, which is greater than the national rate. Homelessness is closely connected to declines in physical and mental health. Persons without homes often lack access to health care and resources for treatment.
Conclusion
The issues and trends discussed in the Mountain View Community summary have their limitations and cannot tell the full story of the health of these counties. Other factors, such as environmental, social and economic, impact individual and community health and provide context necessary to understanding the Community. Therefore, it is important to consider the Social Determinants of Health outlined in this summary when creating plans to address mental health, substance use & recovery, diabetes or any of the other assessed health issues.
Health Services Available
In addition to the websites of participating health systems and public health agencies, there are several robust resource directories available to assist consumers in locating care. These include:










