The Steering Committee determined that Emergency Department (ED) data is essential to the assessment process because it provides current information about the specific communities and populations that are being assessed. It also helps to identify community specific needs, therefore assisting in the creation of the health improvement plans.
The Regional Health Assessment focuses on patients that enter the health systems through the emergency department (ED), because the ED captures patients with all insurance types, including those without insurance. This approach provides the opportunity to assess potential health disparities across patient groups.
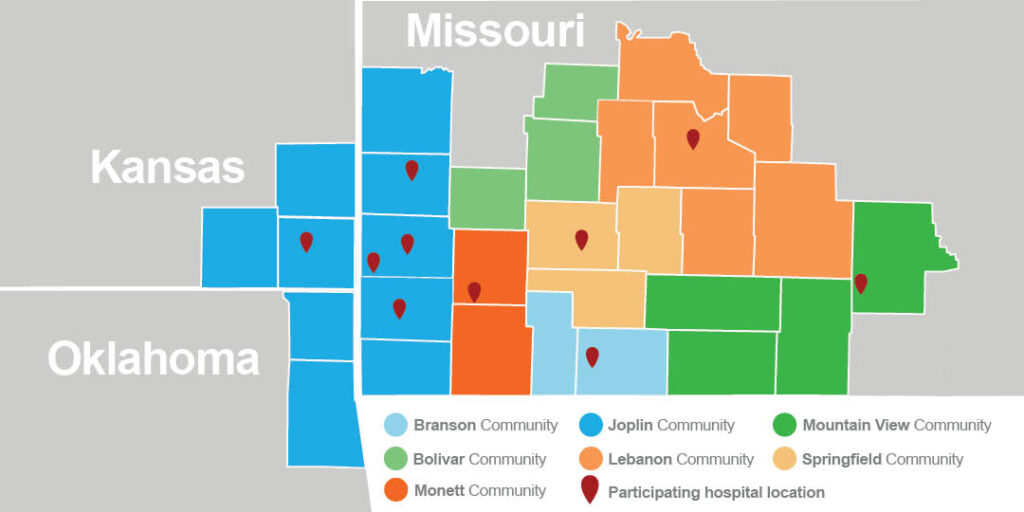
Utilizing their respective organization’s analytics team, data from the three previous calendar years (2018-2020) was collected from each of the following facilities: Cox Barton County Hospital; Cox Medical Center Branson; Cox Medical Center South; Cox North Hospital; Cox Monett Hospital; Freeman Hospital West; Freeman Neosho Hospital; Mercy Hospital Carthage; Mercy Hospital Joplin; Mercy Hospital Columbus: Mercy Hospital Springfield; Mercy Hospital Lebanon; Mercy St. Francis Hospital. International Classification of Diseases, Clinical Modification (ICD-10-CM) diagnosis groups (first three digits only) were used to ensure consistent data collection across facilities that corresponded with pre-determined assessed health issues.
When each hospital finished analysis, analysts at the Springfield Greene County Health Department combined and de-identified the ED data sets in Communities with more than one ED. This approach maintained the collaborative nature of the Regional Health Assessment and provided an insightful perspective of community health needs.
Acknowledging the gaps in other healthcare services proved to the public such as outpatient clinic data is essential. That data could provide this report with a better understanding o the community needs since clinics provide the highest number of patient visits for any community. Future collaborations between hospital systems may provide usable outpatient clinical data that can be aggregated and complied for future assessments.
Key findings
AHI Conditions
- Of the 1,203,465 ED admissions in the Region, 26.3% (316,321) were due to an AHI-related condition, and more than 300,000 ED visits to facilities had diagnoses associated with an AHI.
- Lung Disease was the most frequent diagnosis, comprising 40% of visits attributed to the six AHIs.
- Comparing 2018 (pre-COVID) and 2020 data shows that there was an overall 11% decrease in AHI-related diagnoses during the first year COVID appeared. Lung Disease, 33% decrease
- Cancer, 14% decrease
- Heart Disease, 11% decrease
- Diabetes, 7% decrease
- Mental Health, Substance Use & Recovery, 7% decrease
- COVID-19 was a new diagnosis code introduced in 2020.
Payor Types
- Medicare is the most frequently used payor-type in the OHC Region, used for 37% of AHI-related diagnoses.
- Lung Disease diagnoses are most frequently paid through Medicaid (33%)
- Mental Health, Substance Use & Recovery diagnoses are most frequently paid through Self-Pay (33%)
Demographics
- Men are slightly more likely to present to Springfield’s emergency departments with an AHI-related diagnosis (51% of all visits).
- Males in the Springfield Community have higher rates of emergency department admissions for AHI-related diagnoses with two notable exceptions.
- Females are 15% more likely to be admitted for Diabetes and 16% more likely for Lung Disease- related diagnoses.
- Males are 33% more likely to be admitted for mental health-related diagnoses.
- The majority of those receiving emergency department services for an AHI-related diagnoses in the OHC Region self-identified as Caucasian (89.7%).
- African Americans have the highest rates of admission for each AHI, with the exception of Cancer (where they rank second, after Caucasians).
- Per the graph to the right, admissions for Mental Health and Substance Use Disorder among African Americans is more than double any other race group.
- The oldest members of the OHC Region also have the highest rates of ED admissions for AHI-related diagnoses, with two exceptions.
- Individuals under the age of 18 have the highest admission rate for Lung Disease.
- Those aged 18-64 have the highest admission rates for Mental Health, Substance Use & Recovery (3.7 times higher than those under age 18 and 4.2 times higher than those over age 65.