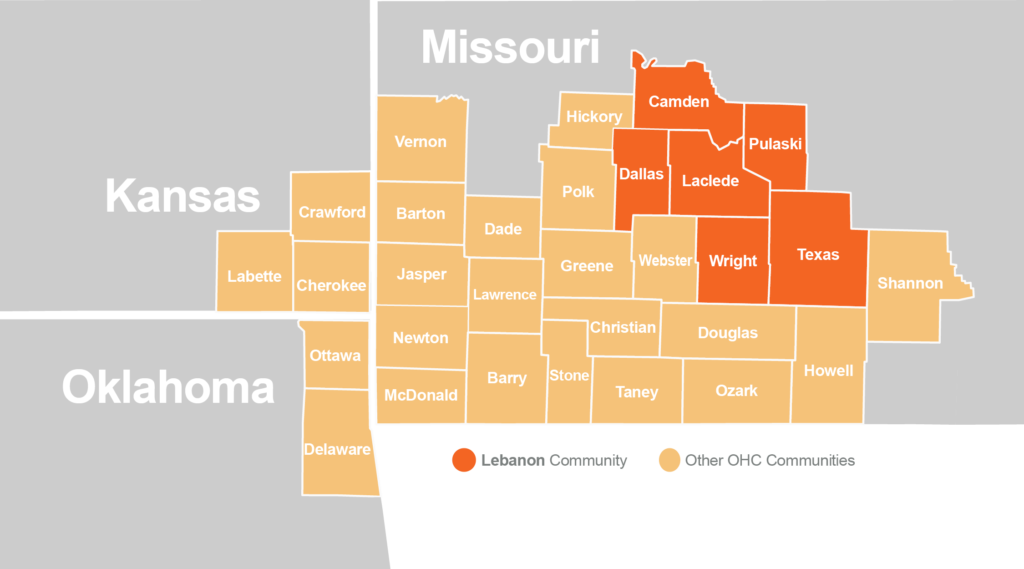
Service Area
The Lebanon Community is made up of 6 counties in Missouri: Laclede, Camden, Dallas, Pulaski, Wright and Texas. The counties included in the Lebanon Community were based on the only participating hospital serving this area, Mercy Hospital Lebanon. The area includes military training bases, rural communities, small townships, a national forest and eight cities, including Lebanon, Waynesville, Houston, Cabool, Mansfield, Hartville, Buffalo and Camdenton.
Lebanon is the Crossroads of the Ozarks, home to over 15,000 residents. Lebanon boasts a diverse economy, including both a regional hospital and a federally qualified health center. The Lebanon motto is “Friendly People, Friendly Place”. Fort Leonard Wood, the military training camp, is home to over 5,000 active duty and over 12,000 family members. In addition, there are other civilian, retirees and family members that live there and thousands of new recruits receive their basic training every year.
Population Overview
The Commission noted several important demographic and population trends within the 6-county Lebanon Community. The 6-county Lebanon Community is home to 193,846 individuals, a decline of 0.5% between 2000 and 2010. A decline in population can cause concerns including aging populations, job losses, declining tax revenues and shrinking schools and neighborhoods.
Nearly 22% of Community residents are minors under the age of 17, while approximately 32% are over the age of 55. Meaning, that the population is, on average, older than both the Region and nation. Older residents are more likely to be living with chronic illnesses and require access to more health services. Further, approximately 60% of the Community is within the age grouping of 18-64, which drives the workforce in the community. Approximately 20% of the total population is living with a disability, which is higher than the regional rate at 17.3% and national rate of 12.62%. This may contribute to access to care and disparities amongst the disability community members. Considerations to consider when planning for improvement in rural versus urban areas. A few of these factors contribute to the overall vulnerability of the population of the Community.
Vulnerable populations, such as people in poverty, minorities, and the elderly, often experience higher rates of chronic illness and worse health outcomes. To ensure vulnerable and at-risk populations were considered when identifying and addressing community health needs, the Commission identified them in each Community using the Center for Disease Control and Prevention (CDC) Social Vulnerability Index (SVI). Using U.S. Census and American Community Survey data, the SVI identifies the most vulnerable groups across all comparative census tracts. Out of the highest vulnerability score of 1.0, the Lebanon Community has an overall SVI score of 0.6, meaning that it is more vulnerable than 60% of the rest of counties in the OHC Region. Scores for Socioeconomic Status (0.7), Household Composition and Disability (0.6), Housing Type and Transportation (0.6), and Minority Status and Language (0.3) demonstrate significant vulnerability of the local population. Homeless students’ status (4.7) is above the OHC region (4.2), Missouri (4.0) and the United States (3.0). This is an area of concern.
What makes a population vulnerable?
| Camden County | Dallas County | Laclede County | Pulaski County | Texas County | Wright County | Lebanon Community | ||
|---|---|---|---|---|---|---|---|---|
| Socio-Economic Status | Below Poverty | 0.48 | 0.34 | 0.34 | 0.3 | 0.93 | 0.94 | 0.56 |
| Unemployed | 0.75 | 0.54 | 0.82 | 0.94 | 0.97 | 0.89 | 0.82 | |
| Income | 0.18 | 0.68 | 0.75 | 0.69 | 0.92 | 0.89 | 0.68 | |
| No High School Diploma | 0.25 | 0.82 | 0.75 | 0.11 | 0.76 | 0.86 | 0.59 | |
| Household Composition & Disability | Aged 65+ | 0.97 | 0.62 | 0.32 | 0 | 0.67 | 0.59 | 0.53 |
| Under Age 18 | 0.04 | 0.79 | 0.82 | 0.34 | 0.25 | 0.87 | 0.52 | |
| Disability Status | 0.7 | 0.82 | 0.63 | 0.75 | 0.89 | 0.73 | 0.75 | |
| Single-Parent Households | 0.03 | 0.69 | 0.34 | 0.4 | 0.63 | 0.89 | 0.5 | |
| Minority Status & Language | Minority | 0.38 | 0.3 | 0.56 | 0.96 | 0.65 | 0.21 | 0.51 |
| Speaks English “Less than Well” | 0.61 | 0.68 | 0.15 | 0.78 | 0.47 | 0.81 | 0.58 | |
| Housing Type & Transportation | Multi-Unit Structures | 1 | 0.29 | 0.64 | 0.82 | 0.35 | 0.45 | 0.59 |
| Mobile Homes | 0.25 | 0.9 | 0.91 | 0.37 | 0.87 | 0.7 | 0.67 | |
| Crowding | 0.36 | 0.86 | 0.92 | 0.39 | 0.39 | 0.95 | 0.65 | |
| No Vehicle | 0.04 | 0.54 | 0.44 | 0.36 | 0.55 | 0.94 | 0.48 | |
| Group Quarters | 0.17 | 0.26 | 0.12 | 0.99 | 0.82 | 0.12 | 0.42 | |
| Orange highlight: The population in this county is more vulnerable than 90% of all other counties in its respective state. | ||||||||
| Blue highlight: The population in this county is more vulnerable than 85% of all other counties in its respective state. | ||||||||
| Beige highlight: The population in this county is more vulnerable than 80% of all other counties in its respective state. | ||||||||
indicative of greater vulnerability. Percentiles are from the CDC’s SVI data.
Assessed Health Issues
Commission stakeholders began the RHA process with analysis of publicly available health data (secondary data) and participating health systems’ emergency room utilization data (primary data) to identify health issues of greatest concern across the region. The result was a ranked list of eight Ozarks Health Commission Region health issues. A full description of the health issues and indicators used can be found in the OHC Regional Health Assessment.
To represent diverse views from across the region and population, qualitative data was garnered. For the Lebanon Community these viewpoints were solicited via 11 individual interviews and 2 focus groups, in addition to the 2,638 surveys collected across the entire OHC Region. Methodologies used for the initial scoring/ranking of the health issues and the full report of the qualitative work can be found in the OHC Regional Report. This prioritization information can be used by organizations to develop community health improvement plans, guide decision making, and foster collaboration across initiatives for collective community impact.
During September and October 2021, three individual interviews, in addition to ten virtual focus group discussions in the Lebanon Community were completed. Those interviewed represented health and social service organizations, education and community collaboratives.
Of the 2,628 survey respondents from the Region, 3.56% indicated they lived in the Lebanon Community. Respondents were asked to rank perceived community needs, and the top 10 that emerged were:
- Drug and other substance abuse treatment and rehabilitation services, including detox
- Emergency mental health services for issues such as suicidal thinking or actions, homicidal thinking or actions, self-harm, or harm to others
- Integrated care, or where people can get medical care and counseling at the same time
- Affordable, quality childcare
- Drug and other substance abuse, education, prevention, and early intervention services
- Coordination of patient care between the hospital and other clinics, private doctors, or others
- Counseling services for mental health issues such as depression, anxiety, trauma, or others for adults
- Counseling services for mental health issues such as depression, anxiety, trauma, or others for adolescents and children
- Affordable housing
- Social services (other than healthcare) for people experiencing homelessness
Those interviewed represented health and social service organizations, education and community collaboratives. Stakeholders, education and community individual interviews and focus groups agreed that a top challenge was access to mental health services and healthcare. This information was considered during the process of establishing health priorities for the Monett Community. Methodologies used for the initial scoring/ranking of the health issues and the full report of the qualitative work can be found in the OHC Regional Report. This prioritization information can be used by organizations to develop community health improvement plans, guide decision-making, and foster collaboration across initiatives.
Lebanon Community Health Priorities
(click a health priority below to learn more)
Each Commission Community convened stakeholders to assess the feasibility of addressing the health issues identified through primary and secondary data sources, and further illuminated the qualitative community feedback. In the Lebanon Community, this was organized by Molly Holtmann, Director of Community Health and Access for Mercy Hospital and was held virtually Thursday, February 3, with every effort made to invite all public health agencies, organizations engaged by Crescendo Consulting, CHC members and leaders of vulnerable and underrepresented communities.
Based on the eight health issues identified by the Commission using publicly available and participating health systems’ data, stakeholders from the Lebanon Community convened to further discuss top priorities for the community.
The feasibility of changing each issue and readiness to address each issue was assessed. Feasibility rankings were influenced by stakeholders’ perceptions of the readiness of the community to address an issue, existing initiatives or momentum, whether leadership was established around the condition, perceived feasibility to change, complexity of the issue and the time frame to improve the issue (within 2-3 years or more than 2-3 years). The higher the score, the more significant the impact of the condition on the community, and the more difficult the condition was to address.
Participants using a short survey, which was opened one week before the meeting, assessed feasibility. Survey responses equaled roughly 50% of the total weighted ranking for each health issue.
| Rank | Initial Ranking Emergency Department and Public Health Data | Final Ranking Emergency Department, Public and Feasibility Data | Rank Change | ||
|---|---|---|---|---|---|
| 1 | Oral Health | 3.44 | COVID-19 | 2.75 | +2 |
| 2 | Lung Disease | 3.23 | Oral Health | 2.64 | -1 |
| 3 | COVID-19 | 2.75 | Lung Disease | 2.48 | -1 |
| 4 | Mental Health | 2.58 | Mental Health | 2.39 | no chante |
| 5 | Heart Disease | 2.56 | Heart Disease | 2.35 | no change |
| 6 | Diabetes | 2.23 | Cancer | 2.13 | +1 |
| 7 | Cancer | 2.14 | Diabetes | 2.08 | -1 |
| 8 | Substance Use & Recovery | 2.04 | Substance Use & Recovery | 2.05 | no change |
Mental Health
Mental health includes a person’s emotional, psychological and social well-being. It affects how individuals think, feel and act. A person’s mental health status also contributes to how they handle stress, relate to others, and make choices. Mental health is important at every stage of life, from childhood and adolescence through adulthood. Many factors contribute to mental health problems, including biology (factors such as genes or brain chemistry), life experiences (such as trauma or abuse) and family history. Within the broad category of mental health, mental illness specifically refers to all diagnosable mental disorders. Mental illness can be chronic or acute. An acute mental health crisis will require different intervention than managing a chronic mental illness.
Homeless teens and homeless in general are a major problem. We have a lot of couch surfers or multifamily homes, not enough homes for the growing community in Lebanon. The number of people without a permanent address is extremely staggering for kids in schools.
Lebanon Community Member
Data used to analyze and prioritize mental health is limited, but it continues to be a topic of great concern among care providers, public health and healthcare partners, media and the community. Although depression is less prevalent in the Lebanon Community, the rate of poor mental health, the number of self-reported poor mental health days in a 30-day period, is higher than in Missouri and the U.S. Moreover, the Lebanon Community has a suicide mortality rate 11% worse than the state average and nearly 50% worse than the national average.
The rate of mental health providers in the Lebanon Community at 36.7 providers per 100,000 residents is slightly lower than the state rate of 37.0 providers per 100,000 Missouri residents. However, 18.3% of adults and 8.2% of children are uninsured in the community. The number of mental health providers is meaningless if those in need cannot access their services. In hospital emergency departments, one in three patients self-paid for services. Concerningly, the second most comment method of payment for mental health related visits was Medicaid, indicating a financial or lifestyle hardship for these patients and how a lack of basic needs can contribute to poor mental health.
Patients that identify as other in the race category in the Lebanon Community visit the emergency department with a mental illness diagnosis at more than five times the rate of any other race group.
The rate of diagnosis for those 18-64 is over 2.5 times higher that of younger residents and that of older residents.
Substance Use & Recovery
Addiction is huge. Suicidal ideation of teenagers is growing, and the internet makes an impact, plus not being in school and no face-to-face interactions. Parents’ addictions, spousal abuse, food insecurity, housing, jobs – all impact behavioral health.
Lebanon Community member
Twenty-two percent of all emergency department visits associated with an assessed health issue were due to mental health or substance use.
Substance use as a behavioral health disorder encompasses the use of intoxicating substances in a manner which negatively effects the persons global wellness. Recovery from substance use disorder is a process through which the individual improves that health and wellness, starts living a self-directed life and striving to reach a more fulfilling purpose. This comes in a variety of pathways, from public health and behavioral health providers, social supports, community resources and mutual aid. There are currently 22.75 million individuals openly in recovery in the US. Only 1 in 4 people needing substance use support and assistance will receive services.
When examining hospital utilization, public health and community input data, substance use and recovery did not rise to top during the prioritization process. After considering that there are significant limitations in collecting and accessing secondary data for this analysis, community stakeholders determined that this assessed health issue was of great priority to the Lebanon Community. Qualitative information shared by both experts and members of the community helps illustrate that there is more of the story missing in the quantitative data.
The Lebanon Community has a substance use prevalence rate that is on par with the rates for entire OHC Region and Missouri and slightly below the U.S. However, the Lebanon Community’s drug poisoning mortality rate is higher than the OHC Region’s rate and the national rate. This is due in large part to Pulaski County’s drug poisoning mortality rate being 36% higher than the state and 59% higher than the national average.
Substance use treatment and rehabilitation services, including detox was the third most important health issue among community input survey respondents, and substance use education, prevention and early intervention ranked ninth. This demonstrates an understanding among the community of the importance of addressing this health issue.
Heart Disease
Heart disease can refer to a variety of conditions that effect the structure or function of the heart. Cardiovascular diseases can be caused or exacerbated by lifestyle choices, other health conditions, age or family history. The two key risk factors for heart disease are high blood pressure and high cholesterol. The Lebanon Community experiences both of these risk factors at greater rates than the entire OHC Region, Missouri, and the U.S.
Several health behaviors can also contribute to poor cardiovascular health and lead to heart disease, with smoking being a significant behavioral risk factor in the Lebanon Community. At 22.6%, the Community has a higher rate of current smokers than the OHC Region, Missouri, and the U.S. Moreover, the rate of poor physical health and obesity in the Lebanon Community are higher than the national rate. This data demonstrates that more can be done to help improve risk factors in the Community by working to change unhealthy behaviors.
Twenty four percent of all emergency department visits associated with an assessed health issue were due to heart disease, making it the second highest diagnosis in hospital visits in the Lebanon Community at 24%.
Sixty three percent of these visits are paid through Medicare, indicating an older population of patients are being admitted through the ER for heart disease.
Special Health Issue: COVID-19
Coronavirus disease (COVID-19) is an infectious disease caused by the SARS-CoV-2 virus. Most people infected with the virus experience mild to moderate respiratory illness and recover without requiring special treatment. However, some become seriously ill and require more advanced medical care. People over the age of 64 and those with underlying medical conditions like cardiovascular disease, diabetes, chronic respiratory disease or cancer are more likely to develop serious illness. Even after recovery, some people may have post-COVID conditions. These conditions can present as different types and combinations of health problems for different lengths of time. Multiorgan effects can affect many body systems, including heart, lung, kidney, skin and neurologic functions.
Isolation is hard, especially for the elderly. When the senior center closed, they lost friends either due to COVID or other illnesses. Churches closed. Expect long-term mental health issues for older adults.
Lebanon Community Member
Throughout the pandemic, the Lebanon Community saw a case rate 2% lower than the state and 8% lower than the national case rate. Two of the six counties in the Community had case rates lower than the state and national averages. However, Laclede County saw a case rate that was 14% higher than Missouri and 7% higher than the U.S.
Despite the overall lower case rate, the Lebanon Community had a rate of mortality from COVID-19 that was more than one-quarter than the state and 11% higher than the nation. Much of this can be attributed to the rate of death from COVID-19 in Laclede County, which saw a mortality rate nearly 90% higher than Missouri and 65% higher than the nation.
COVID-19 was the reason for 3% of emergency department visits in the Lebanon Community, with 46% of patients paying for care through Medicare and 32% utilizing commercial insurance.
Comments from individual interviews and focus groups about the impact of COVID-19 for the community showed concern for the mental health complications from Covid 19. More than half of respondents (all adults) indicate that the COVID-19 pandemic has affected their mental health or the mental health of someone with whom they live, and seven of ten (69.0%) respondents indicate that the mental health of children with whom they live have been impacted.
The COVID-19 pandemic, specifically stemming from low vaccination rates in the area, will have long-lasting effects on many health and social aspects of the population. The Lebanon Community has a vaccination rate 15% lower than the state and 28% lower than the nation rate. According to focus groups, nearly one-third (30.61%) of people who needed care in the past year chose not to receive care, the most common reasons were financial issues (half of those who chose not to seek needed care) and COVID-19-related issues (identified by approximately 28 percent of those who chose not to seek needed care).
Social Determinants of Health
(click a social determinant of health below to learn more)
Additional data critical to understanding the health of the population and the vulnerability of the Community was discerned by examining six groupings classified as social determinants of health: Economic Stability, Education Access and Quality, Healthcare Access and Quality, Neighborhood and Built Environment, Social and Community Context and Health Behaviors. The social determinants of health have a major impact on people’s health, well-being, and quality of life while also contributing widely to health disparities and inequities. Twenty percent of a person’s health and well-being is related to access to care of quality of services provided. Rather, 80% is related to the physical environment (10%), social determinants of health (40%) and health behaviors (30%). Therefore, examination of these factors is important as they play a significant role in the impact the assessed health issues have on the Lebanon Community.
Economic Stability
In the United States, 3 in 10 people live in poverty, and many people can’t afford things like healthy foods, health care, and housing. People with steady employment are less likely to live in poverty and more likely to be healthy, but many people have trouble finding and keeping a job. People with disabilities, injuries, or conditions like arthritis may be especially limited in their ability to work. In addition, many people with steady work still don’t earn enough to afford the things they need to stay healthy.
In the Lebanon Community, 40.6% of residents live at or below 200% of the federal poverty level (FPL), meaning a family of four cannot earn more than $25,750 annually. The percentage of children living in poverty is much higher, at 54.4%.
In addition to living in poverty, many in the Lebanon Community struggle to find affordable housing. More than 26% of those in the Lebanon Community live in substandard housing according to the U.S. Census Bureau and 10.1% report a severe housing cost burden. Thirty-five percent of citizens currently have affordable housing that is below 60% of the area median income (AMI). Community stakeholders note that housing costs in the Lebanon Community have outpaced salaries. There are long wait lists for lower cost rental housing, which is contributing to higher costs.
Education Access & Quality
Education can be an indicator of health, with persons with higher levels of education often living healthier and longer lives. Nearly 13% of adults over 25 years old in the Lebanon Community do not have a high school diploma. Moreover, the Lebanon Community struggles with community members achieving college degrees. Those receiving their associates degree or higher account for 26.9% of the population, which is nearly 30% below the state average and 34% below the national average.
Healthcare Access & Quality
Many people in the United States don’t get the health care services they need. About 1 in 10 people don’t have health insurance. In the Lebanon Community, the rate of uninsured is even higher, with more than 18% of adults and more than 8% of children not having health insurance. People without insurance are less likely to have a primary care provider, and they may not be able to afford the health care services and medications they need. In addition, people may not trust the healthcare system. Some reasons for this may include lack of cultural awareness by providers, feeling unwelcome or uncomfortable in traditional clinical settings, previous negative experiences with healthcare providers, insufficient accommodations for the disabled, language barriers or clinics not having convenient times or locations.
Those with the financial means to access healthcare in the Community have nearly 25 fewer primary care providers per 100,000 residents to seek services with than the rest of Missouri and more than 31 fewer the U.S. Moreover, the Community has slightly fewer mental health care providers than Missouri and more than 35% fewer than the U.S. Overall, the Monett Community struggles with retaining and attracted healthcare providers, with more than 41% of residents living in Health Professional Shortage Areas, a rate that is much higher than the state and national rates.
Input from the community identified healthcare access as a top need and highlighted that people who are trying to make an honest living, the working poor, can’t afford health insurance and other assistance. Only those in extreme poverty can get help.
Health Behaviors
Health behaviors include individual-level behaviors, often influenced by access or quality of services, that can impact the overall health of an individual or community. Measured health behaviors include physical activity, fruit and vegetable expenditures, smoking, alcohol binge drinking, sexually transmitted infection (STI) rates and the prevalence of HIV. These behaviors can affect a wide range of health, functioning, and quality-of-life outcomes and risks.
In the Lebanon Community, physical activity has declined slightly since the prior assessment in 2019. More than one in four (26.2%) residents report no leisure time physical activity, which is higher than both state and national averages.
Analysis of fruit and vegetable expenditures are a way of determining how many community members have the inclination and ability to enjoy healthy foods. In the Lebanon Community, a household spends just over $665 on fruits and vegetables (fresh, frozen, or canned), which is nearly $80 less than the national average.
Additionally, the Lebanon community has a smoking rate slightly higher than the state average, and one-third higher than the national averages.
Neighborhood & Built Environment
The neighborhoods people live in have a major impact on their health and well-being. Where we live affects the basics of our daily lives and health. When affordable housing is lacking it impacts families and where they can afford to live. In the Lebanon Community, more than 26% of community members live in substandard housing. The Community also reports more than one in three community members have limited/low access to food.
Moreover, 26 out of 100 households in the Monett Community have low or slow internet access, a rate higher than the OHC Region, Missouri, and the U.S. As evidenced by the Covid pandemic, this lack of connectivity can affect resident’s ability to learn, work, and play. In Dallas County, only 1 in 3 households have internet that is not low or slow.
Social & Community Context
Health begins where we live, learn and play. Community connections and social relationships can have a major impact on their health and well-being. Many people face challenges and dangers they can’t control, like unsafe neighborhoods, discrimination or trouble affording the things they need. The Lebanon Community has total social vulnerability index (SVI) of 0.6, with 1.0 indicating the highest possible vulnerability. This is 40% higher than both state and national averages. SVI scores that are higher show areas that are more vulnerable to socio-economic factors that can influence their health choices and behaviors. A prime example of this is homelessness. In the Lebanon Community, 4.7% of elementary and secondary students have been identified as homeless, which is greater than the OHC Region, Missouri, and national rates. Homelessness is closely connected to declines in physical and mental health. Persons without homes often lack access to health care and resources for treatment.
Conclusion
The issues and trends discussed in the Lebanon Community summary have their limitations and cannot tell the full story of the health of these counties. Other factors, such as environmental, social and economic, impact individual and community health and provide context necessary to understanding the Community. Therefore, it is important to consider the Social Determinants of Health outlined in this summary when creating plans to address mental health, substance use & recovery, diabetes or any of the other assessed health issues.
Health Services Available
In addition to the websites of participating health systems and public health agencies, there are several robust resource directories available to assist consumers in locating care. These include:
- Burrell Behavioral Health
- Camden County Health Department
- CoxHealth
- Dallas County Health Department
- Jordan Valley Community Health Center
- Laclede County Health Department
- Mercy Hospital Springfield
- Pulaski County Health Department
- Texas County Health Department
- The Arc of the Ozarks
- Wright County Health Department










